Introduction: Why Temperature Monitoring Matters
We all know the feeling, as parents, when our child is warm to the touch and your heart misses a beat. Fever checks become one of our most important parenting skills, and the underarm method is often the safest, easiest choice for children of any ages.
This ultimate guide will take you step by step through all you need to know about using an underarm temperature chart, from the basics to advanced troubleshooting.
Section 1: Understanding Body Temperature Fundamentals
How Body Temperature Works
The human body regulates a fine temperature balance:
- Normal range: 36.5°C-37.5°C (97.7°F-99.5°F)
- Regulated by the hypothalamus (brain’s thermostat)
- Varying during the day (low in the morning, high in the evening).
- Influenced by activity, environment, illness.
Why Underarm Measurement?
Compared to other methods:
- More safer for young children than oral.
- More comfortable than rectal
- More affordable than ear or forehead thermometers
- Works well for all ages, in particular restless toddlers.
Read More:
Underarm Temperature : Unlocking The Role of Your Health
Section 2: The Complete Underarm Temperature Chart
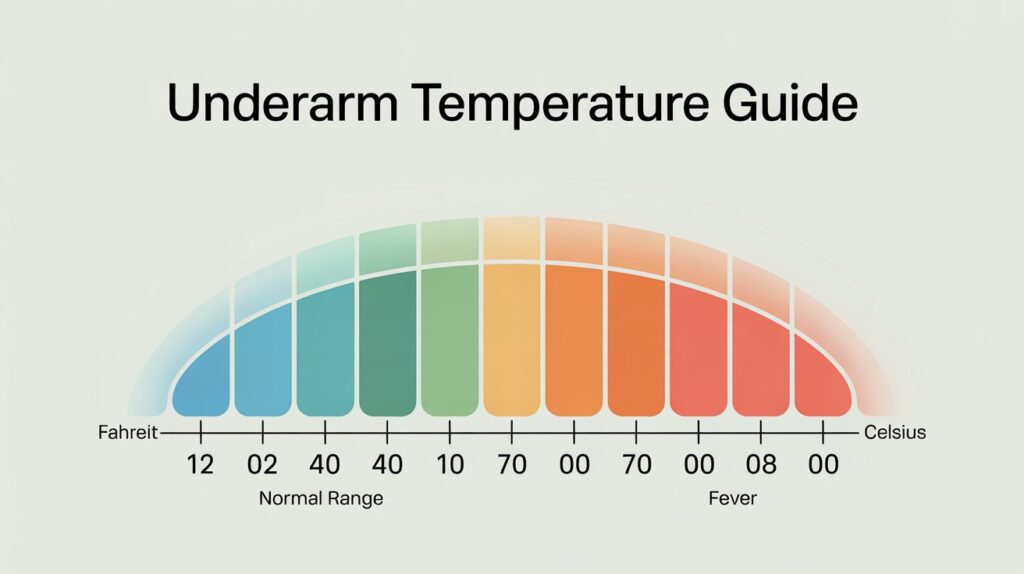
Detailed Temperature Interpretation Guide
| Temperature (°C) | Temperature (°F) | What It Means | Recommended Action |
| Below 36.0°C | Below 96.8°F | Hypothermia risk | Warm child gradually, call doctor if persistent |
| 36.0°C-36.4°C | 96.8°F-97.5°F | Slightly low | Normal for some children, monitor |
| 36.5°C-37.2°C | 97.7°F-99.0°F | Perfectly normal | No action needed |
| 37.3°C-37.5°C | 99.1°F-99.5°F | Slightly elevated | Monitor for changes |
| 37.6°C-38.0°C | 99.7°F-100.4°F | Low-grade fever | Extra fluids, light clothing, monitor |
| 38.1°C-38.5°C | 100.6°F-101.3°F | Moderate fever | Consider fever reducer, call if under 3 months |
| 38.6°C-39.0°C | 101.5°F-102.2°F | High fever | Fever reducer, cool compress, doctor if persists |
| Above 39.0°C | Above 102.2°F | Very high fever | Immediate medical attention for infants |
Temperature Conversion Examples
- 36.9 C to F = 98.4°F (normal)
- 37.5 C to F = 99.5°F (upper normal range)
- 37.7 C to F = 99.9°F (borderline fever)
- 38.2 C to F = 100.8°F (definite fever)
Section 3: Advanced Measurement Techniques
Professional-Grade Measurement Tips
Optimal Positioning
- Center thermometer in armpit
- Ensure good skin contact
- Support arm gently but firmly beside child’s body.
Environmental Factors
- Wait for 15 minutes after entering a cool/ hot place.
- Remove heavy clothing before measuring
- Do not measure immediately after bath or exercise.
Timing Matters
- Best times: Before meals, after quiet time
- Do not measure when crying or very active.
- Regular timing helps in tracking fever patterns.
Troubleshooting Common Issues
- If thermometer will not hold in place: Try to hold child on your lap with their arm against your body.
- For very small infants: Place baby on back, bend arm across chest to hold thermometer.
- With resistant toddlers: Let’s make it a game (Let’s see how warm your superpowers are!).
- When readings seem off: Wait ten minutes and retake making sure of the correct placement.
Section 4: Age-Specific Fever Management
Newborns (0-3 Months)
Special Considerations:
- Immune systems are still developing
- Even fevers that are low can be severe.
- Rectal temps are best but underarm is safer for frequent checks.
Action Plan:
- Call doctor immediately if you have got fever (over 38°C/100.4°F)
- Monitor for other symptoms: poor feeding, unusual sleepiness
- Feed baby often with small amounts to keep him hydrated.
Infants (3-12 Months)
Special Considerations:
- Slight temp increases can be caused by teething.
- More active, more difficult to keep still.
- First fevers usually appear in this stage.
Action Plan:
- For temps 38°C-39°C (100.4°F-102.2°F):
- Offer extra fluids
- Dress lightly
- Take fever reducer if prescribed by doctor.
- Call doctor if:
- Fever lasts more than 24 hours
- Baby is unusually fussy or lethargic.
Toddlers (1-3 Years)
Special Considerations:
- More verbal about discomfort
- Active even when sick
- Frequent minor illnesses build immunity
Action Plan:
- For temps under 38.5°C (101.3°F):
- Focus on comfort
- Encourage rest
- Offer favorite fluids
- For higher temps:
- Appropriate dose of fever reducer
- Lukewarm bath if comfortable
- If fever persists beyond 3 days, call doctor.
Section 5: Comprehensive Fever Care Guide
Creating a Fever Management Kit
Essential items to have ready:
- Digital thermometer (plus backup batteries)
- Fever reducer (pediatrician-approved)
- Measuring syringe or dosing cup
- Hydration options (pedialyte, favorite juice)
- Comfort items (soft washcloths, favorite blanket)
- Temperature log notebook
Step-by-Step Fever Response Plan
- Initial Assessment
- Take temperature properly
- Note time and reading
- Observe other symptoms
- Comfort Measures
- Dress in lightweight clothing
- Keep room comfortably cool
- Give small sips of fluids regularly.
- Medication Decisions
- Use only pediatrician-recommended doses
- Record time given to prevent overdosing.
- Consider alternating medications if advised
- Ongoing Monitoring
- Recheck temp every 2-4 hours
- Watch for behavior changes
- Note wet diapers/urination
Section 6: When to Seek Medical Help
Red Flags Requiring Immediate Attention
- Fever over 40°C (104°F)
- Difficulty breathing
- Stiff neck or severe headache
- Unusual rash
- Seizures or convulsions
- Symptoms of dehydration (no urine for 8+ hours)
Concerning Symptoms Needing Doctor Visit
- Fever lasting more than 3 days
- Fever that disappears and reappears
- Pain with urination
- Pain in ear or pulling at ears
- Unusual sleepiness or irritability
Section 7: Temperature Conversion Master Guide
Complete Conversion Table
| Celsius | Fahrenheit | Significance |
| 36.0°C | 96.8°F | Lower normal |
| 36.5°C | 97.7°F | Ideal normal |
| 37.0°C | 98.6°F | Average normal |
| 37.5°C | 99.5°F | Upper normal |
| 37.6°C | 99.7°F | Beginning fever |
| 38.0°C | 100.4°F | Definite fever |
| 38.5°C | 101.3°F | Moderate fever |
| 39.0°C | 102.2°F | High fever |
| 40.0°C | 104.0°F | Medical emergency |
Quick Conversion Tips
- To convert C to F: Multiply by 1.8, then add 32
- Easy trick: Double the Celsius, subtract 10%, add 32
- Common conversions:
- 37.5 C to F = 99.5°F
- 38.2 C to F = 100.8°F
- 37.7 C to F = 99.9°F
Conclusion: Empowering Parents Through Knowledge
Proficiency in underarm temperature checks is one of the most useful parenting tools you will ever obtain. Remember:
- All is well at 36.9 C to F (98.4°F).
- 37.5 C to F (99.5°F) indicates watchful waiting.
- A temperature of 38.2 C to F (100.8°F) demands action.
With this full guide, you are now able to:
- Take accurate underarm temperatures
- Use our detailed chart to interpret results.
- Respond appropriately to fevers
- Have a feeling for when professional help is needed.
Have this resource ready, believe your parental instincts, and remember – most childhood fevers are short-lived and manageable. You’ve got this!
Section 8: Frequently Asked Questions (Expanded)
Why does my thermometer give different readings each time?
Small variations are normal. Ensure consistent placement, wait between measurements, and consider averaging two readings.
How long should I wait after my child drinks something to take their temperature?
Wait at least 15 minutes after warm or cold drinks for most accurate reading.
My child has 38.2 C to F (100.8°F) but seems fine. Should I worry?
Behavior matters more than the number. If active and drinking well, monitor closely but may not need treatment.
Is alternating acetaminophen and ibuprofen safe?
Only under doctor’s guidance, with careful timing and dose tracking to avoid mistakes.
How accurate are underarm temps compared to rectal?
Typically 0.5°C (1°F) lower. For precise measurement in infants, rectal is gold standard.
Can I use an underarm thermometer for my newborn?
Yes, but add 0.5°C to approximate core temperature, and always verify high readings rectally.
https://shorturl.fm/i264M
https://shorturl.fm/M12Wv
https://shorturl.fm/p7WbQ
https://shorturl.fm/h0Aqs
https://shorturl.fm/03TD8
https://shorturl.fm/ilVjC
https://shorturl.fm/TCvjw
https://shorturl.fm/ClWVb
https://shorturl.fm/PKVMB
https://shorturl.fm/NrxIZ
https://shorturl.fm/U6jRu
https://shorturl.fm/zpbWI
https://shorturl.fm/Q5g0H
https://shorturl.fm/a3FPa
https://shorturl.fm/e4gda
https://shorturl.fm/pABXT
https://shorturl.fm/2ku9f
https://shorturl.fm/F1g7N
https://shorturl.fm/gu6yo
https://shorturl.fm/K5Gr3
https://shorturl.fm/0bBFV
https://shorturl.fm/hExdx
https://shorturl.fm/RNvJS
https://shorturl.fm/JwcwH
https://shorturl.fm/JVqLZ
https://shorturl.fm/amSRr
https://shorturl.fm/ZJ4OR
https://shorturl.fm/Vm34N
https://shorturl.fm/SPbbG
https://shorturl.fm/iFF8F
https://shorturl.fm/1luR1
https://shorturl.fm/ecDA6
https://shorturl.fm/cZqg0
https://shorturl.fm/qxjnH
https://shorturl.fm/0IoSb
https://shorturl.fm/w4SRS
https://shorturl.fm/VL4u7
https://shorturl.fm/DRUl1
https://shorturl.fm/bRMek
https://shorturl.fm/SpcZa
https://shorturl.fm/OstRh
https://shorturl.fm/563W3
https://shorturl.fm/tG4V5
https://shorturl.fm/d1OWW
https://shorturl.fm/iEjEF
https://shorturl.fm/d7edH
https://shorturl.fm/stq0D
https://shorturl.fm/stq0D
https://shorturl.fm/91D16
https://shorturl.fm/RiGIO
https://shorturl.fm/UYUuR
https://shorturl.fm/6e4XO
https://shorturl.fm/phVVR
https://shorturl.fm/hCWOF
https://shorturl.fm/drL4j
https://shorturl.fm/UnESd
https://shorturl.fm/DjZ4P
https://shorturl.fm/wPtto
https://shorturl.fm/WNzym
https://shorturl.fm/1Es0J
https://shorturl.fm/6w3h5
https://shorturl.fm/jcypf
https://shorturl.fm/TS6dI
https://shorturl.fm/PyoyJ
https://shorturl.fm/h1DWt
https://shorturl.fm/1k24Q
https://shorturl.fm/m7iat
https://shorturl.fm/TDlQZ
https://shorturl.fm/iuWJW
https://shorturl.fm/rxnL7
https://shorturl.fm/wbQml
https://shorturl.fm/5GfuE
https://shorturl.fm/Y6pyN
https://shorturl.fm/HciNj
https://shorturl.fm/2jWh1
https://shorturl.fm/HzS5c
https://shorturl.fm/j8EXT
https://shorturl.fm/PG4YA
https://shorturl.fm/e2dv5
https://shorturl.fm/xVuPe
https://shorturl.fm/dumdN
https://shorturl.fm/zH4WF
https://shorturl.fm/2gkEJ
https://shorturl.fm/NCXOu
https://shorturl.fm/qeWWj
https://shorturl.fm/XUP2i
https://shorturl.fm/DoRpL
https://shorturl.fm/kuOl2
https://shorturl.fm/1hBdv
https://shorturl.fm/ATAmi
https://shorturl.fm/t5F6X
https://shorturl.fm/0BsJK
https://shorturl.fm/KG6bH
https://shorturl.fm/NekHG
https://shorturl.fm/xtDbm
https://shorturl.fm/Y4t82
https://shorturl.fm/iOLP1
https://shorturl.fm/l714u
https://shorturl.fm/p1Dn4
https://shorturl.fm/Od3EG
https://shorturl.fm/KqdXw
https://shorturl.fm/pvrlx
https://shorturl.fm/L8tIg
https://shorturl.fm/3VtJP
https://shorturl.fm/47rQC
https://shorturl.fm/kdTYM
https://shorturl.fm/pJBPu
https://shorturl.fm/uibcW
https://shorturl.fm/uLoyR
https://shorturl.fm/eXxAB
https://shorturl.fm/Y4LlC
https://shorturl.fm/1Q7zG